Bulletin - October, 2022
First - the GOOD news...
As we enter the (calendar) months of Spring, we can lay claim to the following:
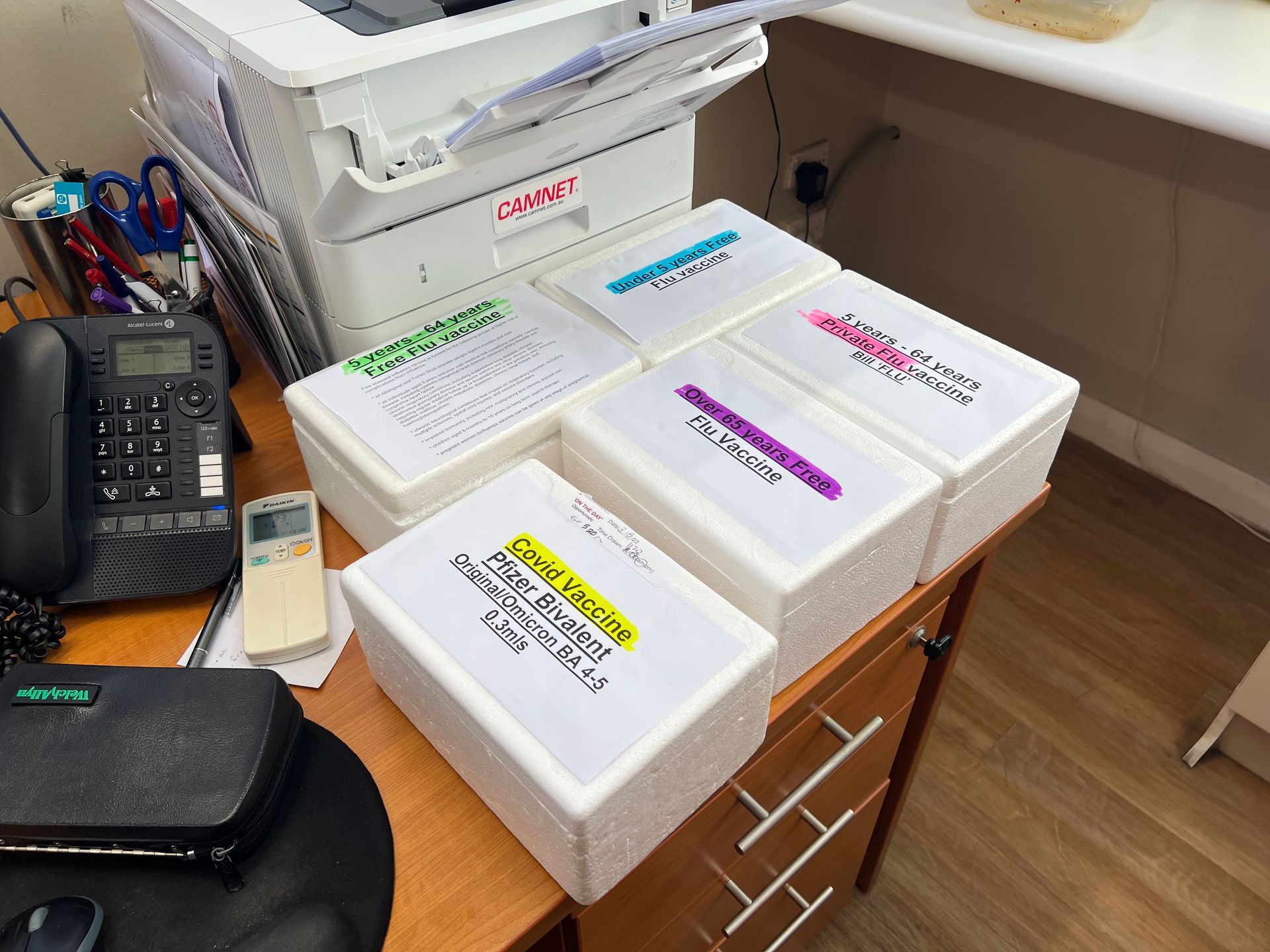
- We've provided more than 2500 flu vaccines since the beginning of the season
- This year alone, we've provided more than 1300 COVID vaccines to the eligible population.
As we've noted previously, despite the vaccine hubs and pharmacies getting behind the program, the vast majority of doses for both influenza and COVID vaccines have been delivered through general practices not unlike ourselves. Given the broad levels of fatigue in the general community, these numbers should not be shrugged off - rather, you all should take some degree of pride in helping to keep our patients safe, or at the very least minimise their risks of severe disease (for both COVID and the flu)!
I'd also like to take a moment to publicly recognise the efforts of our nursing team - Julie Honeychurch and Aimee Martinez for continuing to run clinics and co-ordinate doses throughout this entire ordeal. Thank you both for everything!
...And now, the bad...

The Department of Health and Human Services (DHHS, AKA Medicare) appear to be going through a compliance 'blitz', as are Pharmaceutical Services. In the past two months, the following has occurred:
- The pharmacists at both Newtown Pharmacy and Bob's Chemist have respectively been suspended, with the later being struck from the register due to improper practices regarding the management of schedule 4 and 8 medications and record keeping requirements (both pharmacies are currently operating under new staff.
- A handful of GPs in area have been required to present to Pharmaceutical Services regarding prescribing practices, particularly the absences of proper authority for schedule medications.
In house, there have been a handful of incidents of billing errors that are assumed to be in good faith, where:
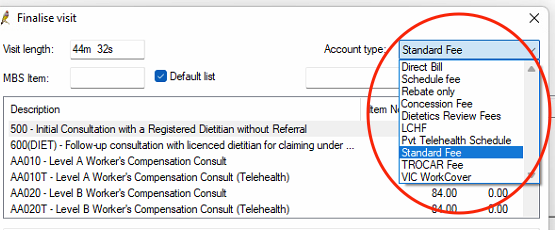
- patients have been billed for in-person attendances when services were provided as telehealth.
- patients have been billed privately for unsolicited telehealth services.
- patients have been billed the concessional attendance item when they are no longer eligible, largely through a quirk in Best Practice's automatic addition of the incentive item (10990) when a concession card number is present.
The responsibility of billing appropriately falls on the shoulders of the individual provider, and so I would ask GPs to be mindful of the items they bill, particularly in this climate of audits. While CSMP does not direct or dictate practitioner billings without the advice of the Doctors' Committee, an audit can create unnecessary anxiety for both GPs and patients, even those not the subject of such an action, so please be mindful in this regard.
In the case of 'unsolicited' telehealth attendances, the majority of these seem to have occurred in the process of routine results follow-up, where the GP has contacted a patient and forgotten to select 'direct bill' rather than 'standard' when finalising the visit. That being said, if a patient is to be billed in this scenario, the GP must obtain the patient's consent to the charge.
As for concessional verification, admin staff have only recently had the capacity to do so returned in Best Practice; any bulk-billed attendance will have the patient's concessional status verified:
- If a patient has a number present and their concessional status is verified, then no action.
- If a patient has a number present and their concessional status fails, the number will be removed and their 'usual billing' type changed from 'Direct Bill' to 'Standard'. In these cases, the patient will either need to present an 'in date' card (if on site), and then contact Centrelink to update their circumstances.
- If a patient has NO number present AND is over 18 years of age, but has a concessional entitlement verified, they'll be asked to present their card to the desk for entry into their demographic records. If they're unable to present the card at the time of their visit, a placeholder number will be entered and a check done monthly to update any 'duplicate' placeholder numbers.
The above only applies to attendances that are 'bulk billed', as the concessional item cannot be privately billed to the patient.
Lastly, all GPs currently have 'Real Time Prescription Monitoring' active in Best Practice, meaning that a pop-up window appears when issuing new prescriptions to patients. This (theoretically) would prevent patients from gaining multiple scripts from different providers across different practices, but not prevent patients from accessing medications that require psychiatric authority unless contraindicated. The list of medications and their authority requirements can be found by clicking below:
Doctors' Committee - position vacant!
With Danielle's departure imminent, there will be a vacant seat on the CSMP Doctors' Committee from February, 2023. The Committee meets once every 2 months on (generally) the second Thursday of the month, to address issues of policy and practice, and acts as a means of presenting the interests of GPs working at CSMP to the service provider.
For more information, please feel free to contact either Anna Connellan or myself - the Committee's remit can be found here:
InstantScripts...
As a direct result of the Pandemic (and to a lesser extent, the accessibility of GPs more widely), a number of organisations have moved into this space to fill perceived gaps in terms of patient's access to care and medications. One such organisation is InstantScripts, which in many fills the role of a Home Doctor Service, without the physical attendance.
However, to meet basic obligations, the provider needs to communicate with a patient's regular GP, which to date, has failed miserably:
If you've seen this message, then you've likely received some 'correspondence' from InstantScripts (I'm working to resolve why this is occurring...the error, that is). While clinical circumstances are obviously unique for each patient, from purely a medico-legal standpoint, this platform raises a number of concerns for patients that are already anxious and vulnerable. In the current season of audits, the fact that we seem to be receiving an increasing amount of correspondence from such a provider is also troubling.
Ultimately, this is clearly a discussion between a GP and their patient, but I'll keep you posted if and when the issue of correspondence is resolved. If you wish to see how the service works, you can click here.
Why we DON'T give patients the practice's email address...
In 2014, CSMP suffered a ransomware attack - if you're not sure what that means, our clinical software was locked, and we were unable to access either patient data, or open any programs, and were told that we had to pay a 'not insignificant' sum for the encryption to be removed.
'Fortunately', the encryption simply 'locked' our access to the data, rather than have a copy downloaded and the privacy and safety of our patients breached. Due to numerous safety processes and data backups, we restored our system in a matter of hours and were able to lock out further cyber threats of a similar nature, at least for the time being.
In 2021, a patient's computer had been infected with a Trojan (a program that is seemingly innocuous, but when opened can have a similar effect to the incident mentioned above) that attempted to download itself over Zoom. This time, as our firewall is adaptive (much like the immune system), the trojan was prevented from downloading itself, and the Zoom program has been quarantined on our firewall since to avoid such an incident happening again.
Unfortunately, these attacks are becoming more sophisticated, and require more aggressive actions be taken to protect both our ability to provide care, but also the sensitive information of our patients. The most recent attacks have come from 'known' senders, such as allied health or operators using their identities, but more often than not patients with poor cyber security on their own systems (one such incident caused the firewall to disconnect the server from the rest of the network to avoid potential infection). Ultimately, we take whatever precautions we can, but the fact is that there is still a very real risk despite these policies and systems.
It's also a fact that organisations that publish their email addresses are far more likely to be the targets of cyber attacks, and so only providing the email address to trusted organisations on demand is one basic security measure that we've taken. The other is to insist that patients use our 'Contact Us' form to submit documents, forms or images, as this provides us with one extra layer of security by passing through an external firewall before arriving at our digital doorstep.
So TL;DR - please do NOT ask patients to email the practice; please ask them to use the appropriate portal, and if they ask why, ask them if they're still with Optus.
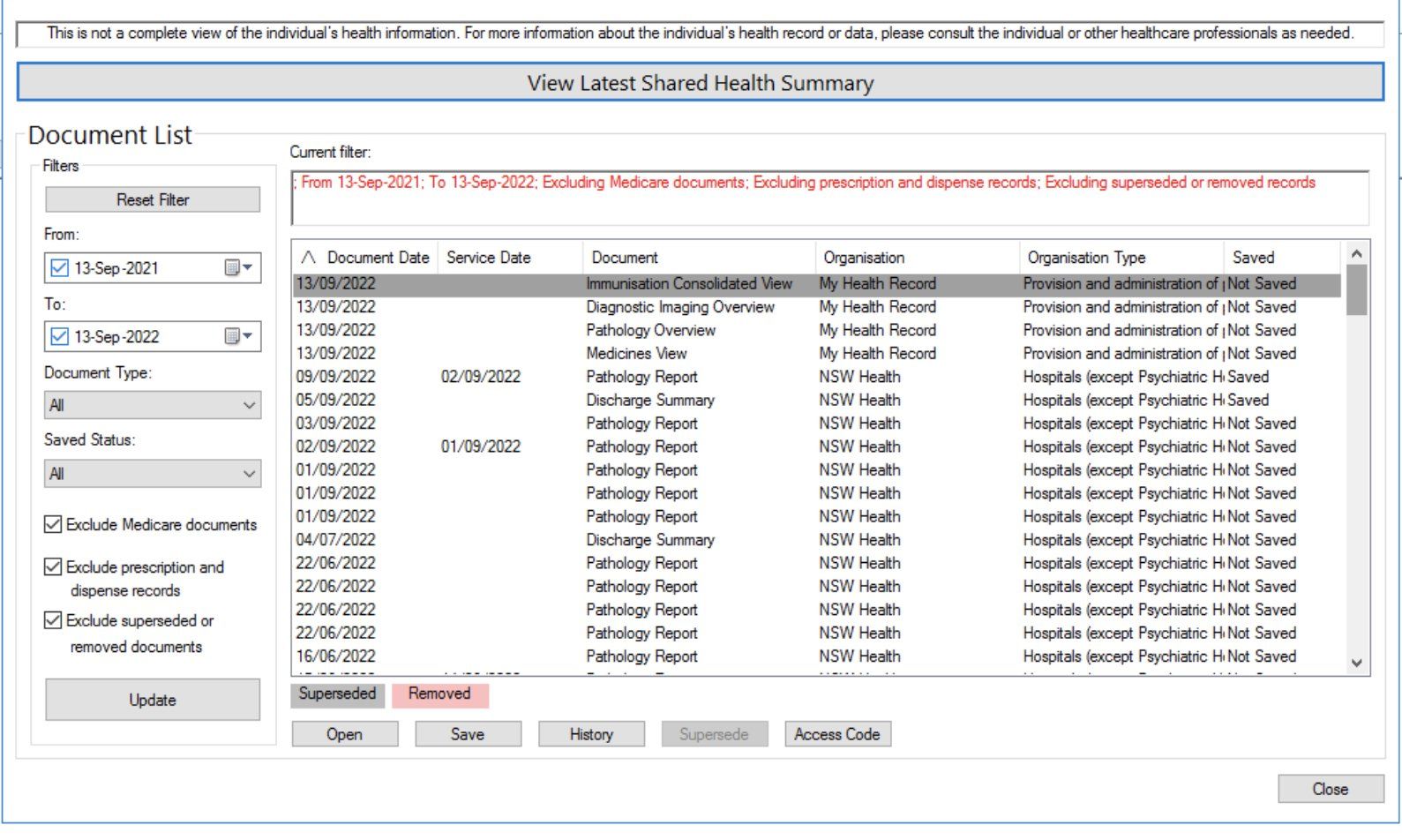
Did You Check the MHR...? (RPT)
While we now have regular and generally reliable access to the National Cancer Screening Registry (NCSR) through Best Practice, a number of pathology providers have begun adding results into patient MHRs - notably Laverty, who have notoriously problematic staff manning the phones should you need to chase a result (record i 40+ mins followed by hanging up).
If you're looking for in-hospital pathology or other results for a patient, please check the MHR first before contacting reception to chase - it may save EVERYONE time!
Coming Events...
- Doctors' Committee - Thursday, 13th October - Room 107, 1-2:30pm. Any agenda items to add, please contact Dr Anna Connellan!
- Moderna Clinics - TBC - For the next phase of our COVID adventure, we'll soon be administering the Moderna Bivalent COVID vaccine. This will require all GPs 'supervising' clinics to have completed the requisite modules, which can be found by clicking HERE.
- uTECH Equipment Calibration - 7th and 14th October. Our annual equipment calibration will take place across the next two Fridays!
- Practice Lunch - Friday, 21st October (1-2:30pm). Bring a plate! With food! Or discover the joys of Uber Eats!
- CSMP Christmas Party - RSVPs are due THIS FRIDAY (7th October)! Please let me know ASAP by clicking HERE!