Eligibility Checks (MHCP)
In order to bill ANY care plan items, you'll need to do the following:
1. Is the Patient eligible?
Before a patient can be billed for a care plan, you'll need to
check their eligibility by logging into the Health Professionals Online Services (HPOS) website:
Once at the site, you'll need to scroll down to log on, by clicking PKI Certificates:
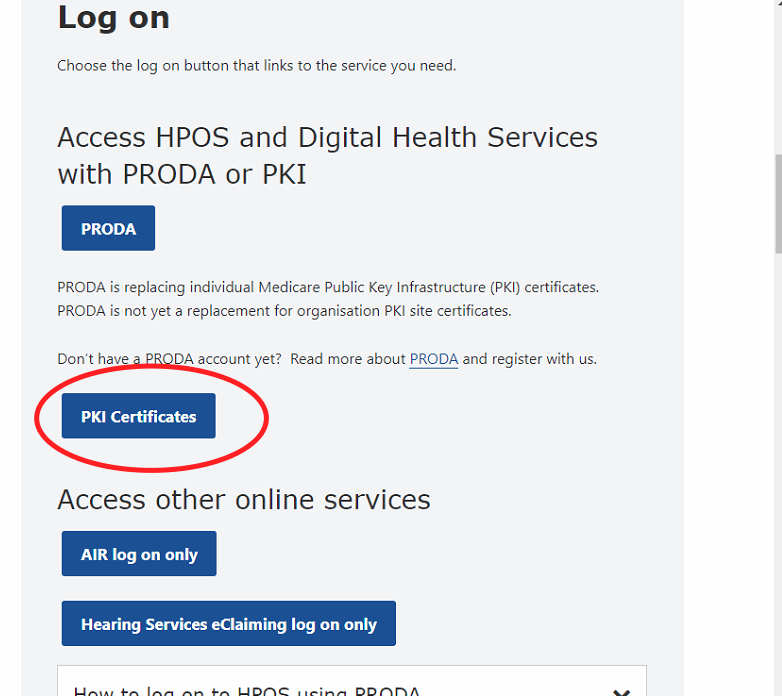
N.B: Before completing this step, you'll need to select the correct PKI certificate for the machine being used, as well as matching password.
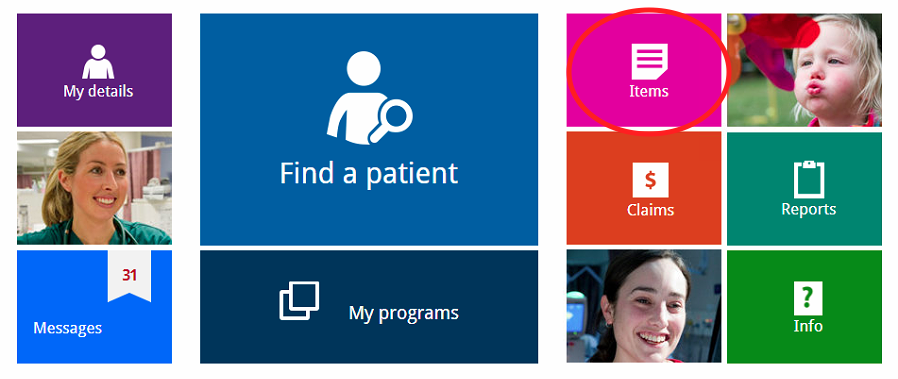
Once logged on, you'll need to select the
Items box:
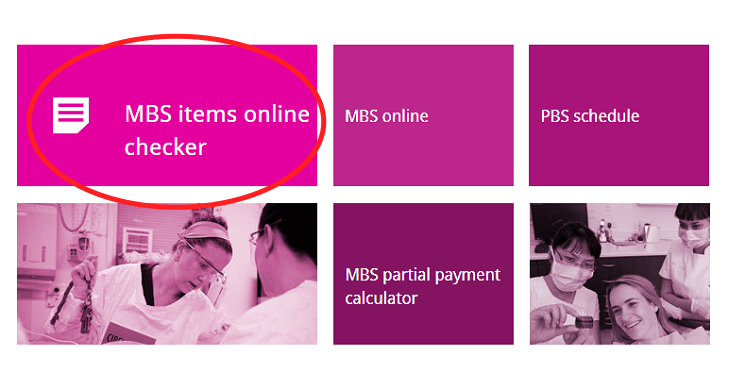
Once here, click on
items, and then select
MBS Items Online Checker:
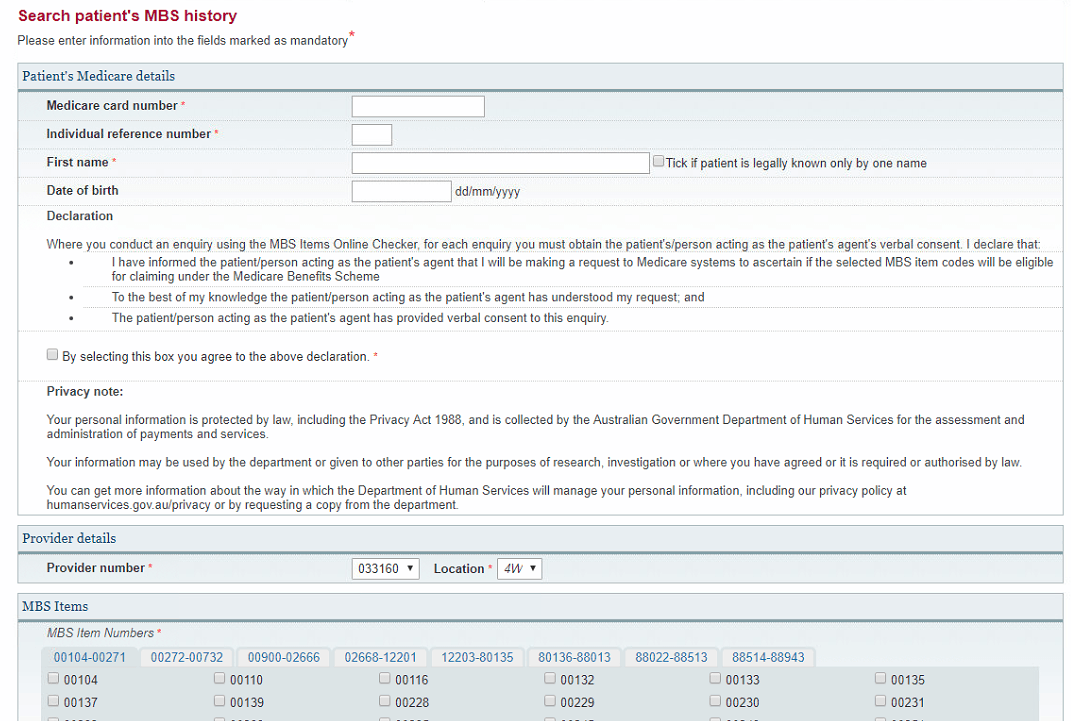
At the next screen, you'll need:
- The Patient's medicare number and card reference number
- The Patient's FIRST name
- To select the RIGHT item numbers to check (you can select a maximum of FIVE (5) items).
- N.B: Because the checker uses base 5 digits, items 2712
and 2715
will appear as:
- 02715
- 02712
Once checked, contact the relevant doctor and let them know their patient's eligibility.
How do the Cycles Work for MHCPs?
For Mental Health Care Plans, the cycle of care would be:
- Initially a 2715/2717 or 2700 or 2701
- A review (2712) after ONE (1) month.
- The NEXT review 3 months after that.
If you're billing a 2712, then the next item would be ANOTHER 2712 in 3 months +1 day's time.
